Nutrition Diva
Nutrition Diva will help you sort food facts from fiction, separate the good information from the bad, and make eating healthy just a little bit easier – and a lot saner.
Listen Now
More From Nutrition Diva
I have another little piece of bonus content for you. A little something extra between our regular episodes of the Nutrition Diva podcast. I really wa...
There’s a new series on Netflix called “You Are What You Eat,” one of a growing number of documentary films advocating for vegan diets. I don’...
Food as medicine: A different approach The notion of food as medicine is certainly nothing new. You’ve probably heard the saying “Let food be ...
Are you participating in Dryuary (or Dry January) this year? If so, you have plenty of company! This month-long observation, in which people commit to...
Nutrition Diva listener Holly wants to know whether mushrooms are a vegetable. And the short answer is: No. But I think we should grant them honorary ...
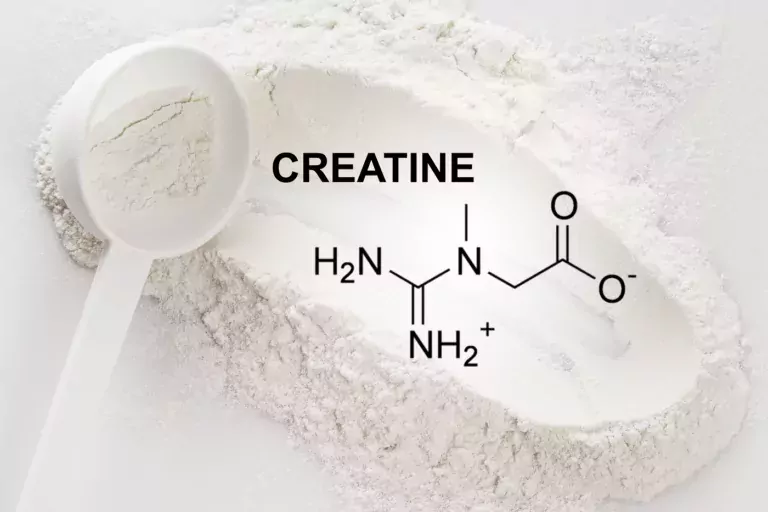
This article, and episode 731 of the podcast (listen in the player above), was prompted by an email from Sandi, who wanted to know if I’d ever done ...
I have gotten a ton of questions recently on a compound called berberine. Is it safe and/or beneficial? So, let’s talk about berberine, a natural co...
Fiber may seem like a somewhat frumpy nutrient, but it is actually one of the hottest nutrition topics right now. That’s partly because fiber plays ...
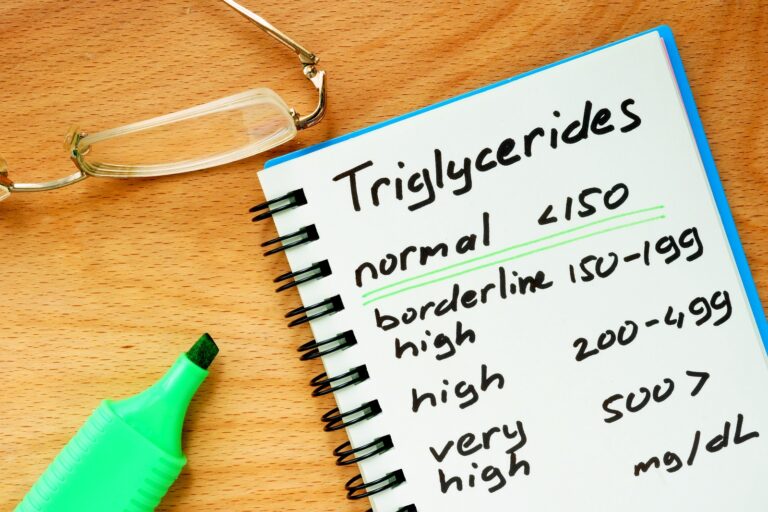
Today we’re going to talk about how to lower high triglycerides. But first, a quick listener Q & A. Ken writes: “Strolling through the far...
I recently had an episode about the difference between powdered cacao and cocoa powder. But the day AFTER that episode was released, Consumer Reports ...
About

Nutrition Diva will help you sort food facts from fiction, separate the good information from the bad, and make eating healthy just a little bit easier – and a lot saner.